Characterization and potential applications of silver nanoparticles: an insight on different mechanisms
Abstract
Keywords
Full Text:
PDFReferences
Wei L, Lu J, Xu H, Patel A, Chen Z-S, Chen G. Silver nanoparticles: synthesis, properties, and therapeutic applications. Drug Discov Today. 2015;20(5):595–601. doi:10.1016/j.drudis.2014.11.014
Zhang X-F, Liu Z-G, Shen W, Gurunathan S. Silver nanoparticles: synthesis, characterization, properties, applications, and therapeutic approaches. Int J Mol Sci. 2016;17(9):E1534. doi:10.3390/ijms17091534
Xu L, Wang Y-Y, Huang J, Chen C-Y, Wang Z-X, Xie H. Silver nanoparticles: synthesis, medical applications and biosafety. Theranostics. 2020;10(20):8996–9031. doi:10.7150/thno.45413
Marin S, Vlascean GM, Tiplea RE, Bucur IR, Lemnaru M, Marin MM, Grumezescu AM. Applications and toxicity of silver nanoparticles: a recent review. Curr Top Med Chem. 2015;15(16):1596–1604. doi:10.2174/1568026615666150414142209
Markowska K, Grudniak AM, Wolska KI. Silver nanoparticles as an alternative strategy against bacterial biofilms. Acta Biochim Pol. 2013;60(4):523–530. doi:10.18388/abp.2013_2016
Tăbăran A-F, Matea CT, Mocan T, Tăbăran A, Mihaiu M, Iancu C, Mocan L. Silver nanoparticles for the therapy of tuberculosis. Int J Nanomed. 2020;15:2231–2258. doi:10.2147/IJN.S241183
Fakhruddin KS, Egusa H, Ngo HC, Panduwawala C, Pesee S, Samaranayake LP. Clinical efficacy and the antimicrobial potential of silver formulations in arresting dental caries: a systematic review. BMC Oral Health. 2020;20(1):160. doi:10.1186/s12903-020-01133-3
Qaralleh H, Khleifat KM, Al-Limoun MO, Alzedaneen FY, Al-Tawarah N. Antibacterial and synergistic effect of biosynthesized silver nanoparticles using the fungi tritirachium oryzae W5H with essential oil of centaurea damascena to enhance conventional antibiotics activity. Adv Nat Sci Nanosci Nanotechnol. 2019;10:025016. doi:10.1088/2043-6254/ab2867
Kaur A, Preet S, Kumar V, Kumar R, Kumar R. Synergetic effect of vancomycin loaded silver nanoparticles for enhanced antibacterial activity. Colloids Surf B Biointerfaces. 2019;176:62–69. doi:10.1016/j.colsurfb.2018.12.043
Hussein EAM, Mohammad AA-H, Harraz FA, Ahsan MF. Biologically synthesized silver nanoparticles for enhancing tetracycline activity against staphylococcus aureus and klebsiella pneumoniae. Braz Arch Biol Technol. 2019;62. doi:10.1590/1678-4324-2019180266
Saha S, Malik MM, Qureshi MS. Study of synergistic effects of antibiotics and triangular shaped silver nanoparticles, synthesized using uv-light irradiation, on s. aureus and p. aeruginosa. Mater Today Proceed. 2019;18:920–927. doi:10.1016/j.matpr.2019.06.525
Farjadian F, Akbarizadeh AR, Tayebi L. Synthesis of novel reducing agent for formation of metronidazolecapped silver nanoparticle and evaluating antibacterial efficiency in gram-positive and gram-negative bacteria. Heliyon. 2020;6(8):e04747. doi:10.1016/j.heliyon.2020.e04747
Gherasim O, Puiu RA, Bîrcă AC, Burdușel A-C, Grumezescu AM. An updated review on silver nanoparticles in biomedicine. Nanomater. 2020;10(11):2318. doi:10.3390/nano10112318
Franci G, Falanga A, Galdiero S, Palomba L, Rai M, Morelli G, Galdiero M. Silver nanoparticles as potential antibacterial agents. Mol. 2015:20(5):8856–8874. doi:10.3390/molecules20058856
Burdușel A-C, Gherasim O, Grumezescu AM, Mogoantă L, Ficai A, Andronescu E. Biomedical applications of silver nanoparticles: an up-to-date overview. Nanomater. 2018:8(9):E681. doi:10.3390/nano8090681
Lubojanski A, Dobrzynski M, Nowak N, Rewak-Soroczynska J, Sztyler K, Zakrzewski W, Dobrzynski W, Szymonowicz M, Rybak Z, Wiglusz K, Wiglusz RJ. Application of selected nanomaterials and ozone in modern clinical dentistry. Nanomater. 2021;11(2):259. doi:10.3390/nano11020259
Guilger-Casagrande M, de Lima R. Synthesis of silver nanoparticles mediated by fungi: a review. Front Bioeng Biotechnol. 2019;7:287. doi:10.3389/fbioe.2019.00287
Dikshit PK, Kumar J, Das AK, Sadhu S, Sharma S, Singh S, Gupta PK, Kim BS. Green Synthesis of Metallic Nanoparticles: Applications and Limitations. Catalysts. 2021;11:902. doi:10.3390/catal11080902
Li W-R, Sun T-L, Zhou S-L, Ma Y-K, Shi Q-S, Xie X, Huang X-M. A comparative analysis of antibacterial activity, dynamics, and effects of silver ions and silver nanoparticles against four bacterial strains. Int Biodeterior Biodegradation. 2017;123. doi:10.1016/j.ibiod.2017.07.015
Galdiero S, Falanga A, Vitiello M, Cantisani M, Marra V, Galdiero M. Silver nanoparticles as potential antiviral agents. Mol. 2011;16(10):8894–8918. doi:10.3390/molecules16108894
Wei Q-Y, He K-M, Chen J-L, Xu Y-M, Lau ATY. Phytofabrication of nanoparticles as novel drugs for anticancer applications. Mol. 2019;24(23):4246. doi:10.3390/molecules24234246
Acosta-Torres LS, Mendieta I, Nuñez-Anita RE, Cajero-Juárez M, Castaño VM. Cytocompatible antifungal acrylic resin containing silver nanoparticles for dentures. Int J Nanomed. 2012;7:4777–4786. doi:10.2147/IJN.S32391
Panáček A, Kvítek L, Smékalová M, Večeřová R, Kolář M, Röderová M, Dyčka F, Šebela M, Prucek R, Tomanec O, Zbořil R. Bacterial resistance to silver nanoparticles and how to overcome it. Nat Nanotechnol. 2018;13(1):65–71. doi:10.1038/s41565-017-0013-y
Asadishad B, Hidalgo G, Tufenkji N. Pomegranate materials inhibit flagellin gene expression and flagellar-propelled motility of uropathogenic escherichia coli strain CFT073. FEMS Microbiol Lett. 2012;334(2):87–94. doi:10.1111/j.1574-6968.2012.02622.x
Baethge C, Goldbeck-Wood S, Mertens S. SANRAa scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4:5. Published 2019 Mar 26. doi:10.1186/s41073-019-0064-8
Agnihotri S, Mukherji S, Mukherji S. Size-controlled silver nanoparticles synthesized over the range 5–100 nm using the same protocol and their antibacterial efficacy. RSC Adv. 2013;4(8):3974–3983. doi:10.1039/C3RA44507K
Baker C, Pradhan A, Pakstis L, Pochan D, Shah S. Synthesis and antibacterial properties of silver nanoparticles. J Nanosci Nanotechnol. 2005;5:244–249. doi:10.1166/jnn.2005.034
Liu J, Hurt RH. Ion release kinetics and particle persistence in aqueous nanosilver colloids. Environ Sci Technol. 2010;44(6):2169–2175. doi:10.1021/es9035557
Sotiriou GA, Pratsinis SE. Antibacterial activity of nanosilver ions and particles. Environ Sci Technol. 2010;44(14):5649–5654. doi:10.1021/es101072s
Dobias J, Bernier-Latmani R. Silver release from silver nanoparticles in natural waters. Environ Sci Technol. 2013;47(9):4140–4146. doi:10.1021/es304023p
Morones JR, Elechiguerra JL, Camacho A, Holt K, Kouri JB, Ramírez JT, Yacaman MJ. The bactericidal effect of silver nanoparticles. Nanotechnol. 2005;16(10):2346–2353. doi:10.1088/0957-4484/16/10/059
Radzig MA, Nadtochenko VA, Koksharova OA, Kiwi J, Lipasova VA, Khmel IA. Antibacterial effects of silver nanoparticles on gram-negative bacteria: influence on the growth and biofilms formation, mechanisms of action. Colloids Surf B Biointerfaces. 2013;102:300–306. doi:10.1016/j.colsurfb.2012.07.039
Bélteky P, Rónavári A, Zakupszky D, Boka E, Igaz N, Szerencsés B, Pfeiffer I, Vágvölgyi C, Kiricsi M, Kónya Z. Are smaller nanoparticles always better? Understanding the biological effect of size-dependent silver nanoparticle aggregation under biorelevant conditions. Int J Nanomed. 2021;16:3021–3040. doi:10.2147/IJN.S304138
Levard C, Hotze EM, Lowry GV, Brown GE. Environmental transformations of silver nanoparticles: impact on stability and toxicity. Environ Sci Technol. 2012;46(13):6900–6914. doi:10.1021/es2037405
Ringe E, Zhang J, Langille M, Mirkin C, Marks L, Duyne R. Correlating the structure and localized surface plasmon resonance of single silver right bipyramids. Nanotechnol. 2012;23:444005. doi:10.1088/0957-4484/23/44/444005
Liu G, Eichelsdoerfer DJ, Rasin B, Zhou Y, Brown KA, Liao X, Mirkin CA. Delineating the pathways for the site-directed synthesis of individual nanoparticles on surfaces. Proceed Nat Acad Sci. 2013;110(3):887–891. doi:10.1073/pnas.1220689110
Wiley B, Sun Y, Xia Y. Synthesis of silver nanostructures with controlled shapes and properties. Acc Chem Res. 2007;40(10):1067–1076. doi:10.1021/ar7000974
Pal S, Tak YK, Song JM. Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A Study of the gram-negative bacterium escherichia coli. Appl Environ Microbiol. 2007;73(6):1712–1720. doi:10.1128/AEM.02218-06
Cheon JY, Kim SJ, Rhee YH, Kwon OH, Park WH. Shape-dependent antimicrobial activities of silver nanoparticles. Int J Nanomed. 2019;14:2773–2780. doi:10.2147/IJN.S196472
Helmlinger J, Sengstock C, Groß-Heitfeld C, Mayer C, Schildhauer TA, Köller M, Epple M. Silver nanoparticles with different size and shape: equal cytotoxicity, but different antibacterial effects. RSC Adv. 2016;6(22):18490–18501. doi:10.1039/C5RA27836H
Alshareef A, Laird K, Cross RBM. Shape-dependent antibacterial activity of silver nanoparticles on escherichia coli and enterococcus faecium bacterium. Appl Surf Sci. 2017;424:310–315. doi:10.1016/j.apsusc.2017.03.176
Lee SH, Jun BH. Silver Nanoparticles: Synthesis and Application for Nanomedicine. Int J Mol Sci. 2019;20(4):865. doi:10.3390/ijms20040865
Zhang C, Hu Z, Deng B. Silver nanoparticles in aquatic environments: physiochemical behavior and antimicrobial mechanisms. Water Res. 2016;88:403–427. doi:10.1016/j.watres.2015.10.025
Mackay ME, Dao TT, Tuteja A, Ho DL, van Horn B, Kim H-C, Hawker CJ. Nanoscale effects leading to non-einstein-like decrease in viscosity. Nat Mater. 2003;2(11):762–766. doi:10.1038/nmat999
Zhang W, Yao Y, Li K, Huang Y, Chen Y. Influence of dissolved oxygen on aggregation kinetics of citrate-coated silver nanoparticles. Environ Pollut. 2011;159(12):3757–3762. doi:10.1016/j.envpol.2011.07.013
Panáček A, Kvítek L, Prucek R, Kolář M, Večeřová R, Pizúrová N, Sharma VK, Nevěčná T, Zbořil R. Silver colloid nanoparticles: synthesis, characterization, and their antibacterial activity. J Phys Chem B. 2006;110(33):16248–16253. doi:10.1021/jp063826h
Shu M, He F, Li Z, Zhu X, Ma Y, Zhou Z, Yang Z, Gao F, Zeng M. Biosynthesis and antibacterial activity of silver nanoparticles using yeast extract as reducing and capping agents. Nanoscale Res Lett. 2020;15(1):14. doi:10.1186/s11671-019-3244-z
Ugwoke E, Aisida SO, Mirbahar AA, Arshad M, Ahmad I, Zhao T, Ezema FI. Concentration induced properties of silver nanoparticles and their antibacterial study. Surf Interfaces. 2020;18:100419. doi:10.1016/j.surfin.2019.100419
Ajitha B, Reddy YAK, Reddy PS, Jeon H-J, Ahn CW. Role of capping agents in controlling silver nanoparticles size, antibacterial activity and potential application as optical hydrogen peroxide sensor. RSC Adv. 2016;6(42):36171–36179. doi:10.1039/C6RA03766F
Li Y, Zhang W, Niu J, Chen Y. Surface-coating-dependent dissolution, aggregation, and reactive oxygen species (ROS) generation of silver nanoparticles under different irradiation conditions. Environ Sci Technol. 2013;47(18):10293–10301. doi:10.1021/es400945v
Kim KD, Han D, Kim H. Optimization of experimental conditions based on the taguchi robust design for the formation of nanosized silver particles by chemical reduction method. 2004. doi:10.1016/J.CEJ.2004.08.003
Sharma VK, Siskova KM, Zboril R, Gardea-Torresdey JL. Organic-coated silver nanoparticles in biological and environmental conditions: fate, stability and toxicity. Adv Colloid Interface Sci. 2014;204:15–34. doi:10.1016/j.cis.2013.12.002
Loza K, Diendorf J, Sengstock C, Ruiz-Gonzalez L, Gonzalez-Calbet JM, Vallet-Regi M, Köller M, Epple M. The dissolution and biological effects of silver nanoparticles in biological media. J Mater Chem B. 2014;2(12):1634–1643. doi:10.1039/C3TB21569E
Mitra C, Gummadidala M, Afshinnia K, Merrifield RC, Baalousha M, Lead JR, Chanda A. Citrate-coated silver nanoparticles growth-independently inhibit aflatoxin synthesis in aspergillus parasiticus. Environ Sci Technol. 2017;51(14):8085–8093. doi:10.1021/acs.est.7b01230
Shrivas K, Sahu B, Deb MK, Thakur SS, Sahu S, Kurrey R, Kant T, Patle TK, Jangde R. Colorimetric and paper-based detection of lead using pva capped silver nanoparticles: experimental and theoretical approach. Microchem J. 2019;150. doi:10.1016/j.microc.2019.104156
Rezaei H, Rahimpour E, Khoubnasabjafari M, Jouyban-Gharamaleki V, Jouyban A. A colorimetric nanoprobe based on dynamic aggregation of sds-capped silver nanoparticles for tobramycin determination in exhaled breath condensate. Microchim Acta. 2020;187. doi:10.1007/s00604-020-4162-6
Kamarudin D, Hashim NA, Ong BH, Che Hassan CR, Abdul Manaf N. Synthesis of silver nanoparticles stabilised by pvp for polymeric membrane application: a comparative study. Mat Technol. 2022;37(5):289–301. doi:10.1080/10667857.2021.1908768
Kubo A-L, Capjak I, Vrček IV, Bondarenko OM, Kurvet I, Vija H, Ivask A, Kasemets K, Kahru A. Antimicrobial potency of differently coated 10 and 50 nm silver nanoparticles against clinically relevant bacteria escherichia coli and staphylococcus aureus. Colloids Surf B Biointerfaces. 2018;170:401–410. doi:10.1016/j.colsurfb.2018.06.027
Leo BF, Chen S, Kyo Y, Herpoldt KL, Terrill NJ, Dunlop IE, McPhail DS, Shaffer MS, Schwander S, Gow A, Zhang J, Chung KF, Tetley TD, Porter AE, Ryan MP. The stability of silver nanoparticles in a model of pulmonary surfactant. Environ Sci Technol. 2013;47(19):11232–11240. doi:10.1021/es403377p
Kvítek L, Panáček A, Soukupová J, Kolář M, Večeřová R, Prucek R, Holecová M, Zbořil R. Effect of surfactants and polymers on stability and antibacterial activity of silver nanoparticles (NPs). J Phys Chem C. 2008;112(15):5825–5834. doi:10.1021/jp711616v
Roy A, Bulut O, Some S, Mandal AK, Yilmaz MD. Green synthesis of silver nanoparticles: biomolecule-nanoparticle organizations targeting antimicrobial activity. RSC Adv. 2019;9(5):2673–2702. doi:10.1039/C8RA08982E
Tripathi RM, Chung SJ. Biogenic nanomaterials: synthesis, characterization, growth mechanism, and biomedical applcations. J Microbiol Method. 2019;157:65–80. doi:10.1016/j.mimet.2018.12.008
Hamouda RA, Hussein MH, Aboelmagd RA, Bawazir SS. Synthesis and biological characterization of silver nanoparticles derived from the cyanobacterium oscillatoria limnetica. Sci Rep. 2019;9(1):13071. doi:10.1038/s41598-019-49444-y
Siddiqi KS, Husen A, Rao RAK. A review on biosynthesis of silver nanoparticles and their biocidal properties. J Nanobiotechnol. 2018;16(1):14. doi:10.1186/s12951-018-0334-5
Begum NA, Mondal S, Basu S, Laskar RA, Mandal D. Biogenic synthesis of Au and Ag nanoparticles using aqueous solutions of black tea leaf extracts. Colloids Surf B Biointerfaces. 2009;71(1):113–118. doi:10.1016/j.colsurfb.2009.01.012
Loo, Y. Y, Chieng, B. W, Nishibuchi, M, Radu, S. Synthesis of silver nanoparticles by using tea leaf extract from camellia sinensis. Int J Nanomed. 2012;7:4263–4267. doi:10.2147/IJN.S33344
Rai M, Bonde S, Golinska P, et al. Fusarium as a Novel Fungus for the Synthesis of Nanoparticles: Mechanism and Applications. J Fungi (Basel). 2021;7(2):13915. doi:10.3390/jof7020139
Konappa N, Udayashankar AC, Dhamodaran N, Krishnamurthy S, Jagannath S, Uzma F, Pradeep CK, De Britto S, Chowdappa S, Jogaiah S. Ameliorated antibacterial and antioxidant properties by trichoderma harzianum mediated green synthesis of silver nanoparticles. Biomol. 2021;11(4):535. doi:10.3390/biom11040535
Cheng F, Betts JW, Kelly SM, Hector AL. Green Synthesis of highly concentrated aqueous colloidal solutions of large starch-stabilised silver nanoplatelets. Mater Sci Eng C Mater Biol Appl. 2015;46:530–537. doi:10.1016/j.msec.2014.10.041
Skiba MI, Vorobyova VI, Pivovarov A, Makarshenko NP. Green synthesis of silver nanoparticles in the presence of polysaccharide: optimization and characterization. J Nanomat. 2020;e3051308. doi:10.1155/2020/3051308
Gopinath V, MubarakAli D, Vadivelu J, Manjunath Kamath S, Syed A, Elgorban AM. Synthesis of biocompatible chitosan decorated silver nanoparticles biocomposites for enhanced antimicrobial and anticancer property. Process Biochem. 2020;99:348–356. doi:10.1016/j.procbio.2020.09.011
Muhammad Tahir H, Saleem F, Ali S, Ain Q, Fazal A, Summer M, Mushtaq R, Tariq Zahid M, Liaqat I, Murtaza G. Synthesis of sericin-conjugated silver nanoparticles and their potential antimicrobial activity. J Basic Microbiol. 2020;60(5):458–467. doi:10.1002/jobm.201900567
Azócar MI, Alarcón R, Castillo A, Blamey JM, Walter M, Paez M. Capping of silver nanoparticles by antiinflammatory ligands: antibacterial activity and superoxide anion generation. J Photochem Photobiol B. 2019;193:100–108. doi:10.1016/j.jphotobiol.2019.02.005
Lee, K. J, Browning, L. M, Nallathamby, P. D, Xu, X.-H. N. Study of charge-dependent transport and toxicity of peptide-functionalized silver nanoparticles using zebrafish embryos and single nanoparticle plasmonic spectroscopy. Chem Res Toxicol. 2013;26(6):904–917. doi:10.1021/tx400087d
Abbaszadegan A, Ghahramani Y, Gholami A, Hemma-teenejad B, Dorostkar S, Nabavizadeh M, Sharghi H. The effect of charge at the surface of silver nanoparticles on antimicrobial activity against gram-positive and gram-negative bacteria: a preliminary study. J Nanomat. 2015;e720654. doi:10.1155/2015/720654
Silhavy TJ, Kahne D, Walker S. The bacterial cell envelope. cold spring harbor perspectives in biology. 2010;2(5). doi:10.1101/cshperspect.a000414
El Badawy AM, Silva RG, Morris B, Scheckel KG, Suidan MT, Tolaymat TM. Surface charge-dependent toxicity of silver nanoparticles. Environ Sci Technol. 2011;45(1):283–287. doi:10.1021/es1034188
Qiao Z, Yao Y, Song S, Yin M, Luo J. Silver nanoparticles with ph induced surface charge switchable properties for antibacterial and antibiofilm applications. J Mater Chem B. 2019;7(5):830–840. doi:10.1039/C8TB02917B
Stebounova LV, Guio E, Grassian VH. Silver nanoparticles in simulated biological media: a study of aggregation, sedimentation, and dissolution. J Nanoparticle Res. 2011;13:233–244. doi:10.1007/s11051-010-0022-3
Zhou W, Liu Y-L, Stallworth AM, Ye C, Lenhart JJ. Effects of pH, electrolyte, humic acid, and light exposure on the longterm fate of silver nanoparticles. Environ Sci Technol. 2016;50(22):12214–12224. doi:10.1021/acs.est.6b03237
McShan D, Ray PC, Yu H. Molecular toxicity mechanism of nanosilver. J Food Drug Anal. 2014;22(1):116–127. doi:10.1016/j.jfda.2014.01.010
Bélteky P, Rónavári A, Igaz N, Szerencsés B, Tóth IY, Pfeiffer I, Kiricsi M, Kónya Z. Silver nanoparticles: aggregation behavior in biorelevant conditions and its impact on biological activity. Int J Nanomed. 2019;14:667–687. doi:10.2147/IJN.S185965
Gorshkov V, Bubis JA, Solovyeva EM, Gorshkov MV, Kjeldsen F. Protein corona formed on silver nanoparticles in blood plasma is highly selective and resistant to physicochemical changes of the solution. Environ Sci Nano. 2019;6(4):1089–1098. doi:10.1039/C8EN01054D
Schöttler S, Landfester K, Mailänder V. Controlling the stealth effect of nanocarriers through understanding the protein corona. Angew Chem Int Ed Engl. 2016;55(31):8806–8815. doi:10.1002/anie.201602233
Lundqvist M, Stigler J, Elia G, Lynch I, Cedervall T, Dawson KA. Nanoparticle size and surface properties determine the protein corona with possible implications for biological impacts. Proc Nat Acad Sci USA. 2008;105(38):14265–14270. doi:10.1073/pnas.0805135105
Tenzer S, Docter D, Rosfa S, Wlodarski A, Kuharev J, Rekik A, Knauer SK, Bantz C, Nawroth T, BierC, Sirirattanapan J, Mann W, Treuel L, Zellner R, Maskos M, Schild H, Stauber RH. Nanoparticle size is a critical physicochemical determinant of the human blood plasma corona: a comprehensive quantitative proteomic analysis. ACS Nano. 2011;5(9):7155–7167. doi:10.1021/nn201950e
Tai J-T, Lai C-S, Ho H-C, Yeh Y-S, Wang H-F, Ho R-M, Tsai D-H. Protein-silver nanoparticle interactions to colloidal stability in acidic environments. Langmuir. 2014;30(43):12755–12764. doi:10.1021/la5033465
Alarcon E, Bueno-Alejo C, Noel C, Stamplecoskie K, Pacioni N, Poblete H, Scaiano JC. Human serum albumin as protecting agent of silver nanoparticles: role of the protein conformation and amine groups in the nanoparticle stabilization. J Nanoparticle Res. 2013;15:1–14. doi:10.1007/s11051-012-1374-7
Bhargava A, Dev A, Mohanbhai SJ, Pareek V, Jain N, Choudhury SR, Panwar J, Karmakar S. Pre-coating of protein modulate patterns of corona formation, physiological stability and cytotoxicity of silver nanoparticles. Sci Total Environ. 2021;772:144797. doi:10.1016/j.scitotenv.2020.144797
Walkey CD, Olsen JB, Song F, Liu R, Guo H, Olsen DWH, Cohen Y, Emili A, Chan WCW. Protein corona fingerprinting predicts the cellular interaction of gold and silver nanoparticles. ACS Nano. 2014;8(3):2439–2455. doi:10.1021/nn406018q
Fernando I, Zhou Y. Impact of pH on the stability, dissolution and aggregation kinetics of silver nanoparticles. Chemosphere. 2019;216:297–305. doi:10.1016/j.chemosphere.2018.10.122
Sivera M, Kvitek L, Soukupova J, Panacek A, Prucek R, Vecerova R, Zboril R. Silver nanoparticles modified by gelatin with extraordinary pH stability and long-term antibacterial activity. PLOS ONE. 2014;9(8):e103675. doi:10.1371/journal.pone.0103675
Choi O, Clevenger TE, Deng B, Surampalli RY, Ross L, Hu Z. Role of sulfide and ligand strength in controlling nanosilver toxicity. Water Res. 2009;43(7):1879–1886. doi:10.1016/j.watres.2009.01.029
Zhang Y, Chen Y, Westerhoff P, Crittenden J. Impact of natural organic matter and divalent cations on the stability of aqueous nanoparticles. Water Res. 2009;43(17):4249–4257. doi:10.1016/j.watres.2009.06.005
Baalousha M, Nur Y, Römer I, Tejamaya M, Lead JR. Effect of monovalent and divalent cations, anions and fulvic acid on aggregation of citrate-coated silver nanoparticles. Sci Total Environ. 2013;454–455:119–131. doi:10.1016/j.scitotenv.2013.02.093
Harmon AR, Kennedy AJ, Poda AR, Bednar AJ, Chappell MA, Steevens JA. Determination of nanosilver dissolution kinetics and toxicity in an environmentally relevant aqueous medium. Environ Toxicol Chem. 2014;33(8):1783–1791. doi:10.1002/etc.2616
Fan X, Yahia L, Sacher E. Antimicrobial properties of the ag, cu nanoparticle system. Biol. 2021;10(2):137. doi:10.3390/biology10020137
Salleh A, Naomi R, Utami ND, Mohammad AW, Mahmoudi E, Mustafa N, Fauzi MB. The potential of silver nanoparticles for antiviral and antibacterial applications: a mechanism of action. Nanomater. 2020;10(8):1566. doi:10.3390/nano10081566
Vazquez-Muñoz R, Meza-Villezcas A, Fournier PGJ, Soria-Castro E, Juarez-Moreno K, Gallego-Hernández AL, Bog-danchikova N, Vazquez-Duhalt R, Huerta-Saquero A. En-hancement of antibiotics antimicrobial activity due to the silver nanoparticles impact on the cell membrane. PLoS One. 2019;14(11):e0224904. doi:10.1371/journal.pone.0224904
Li W-R, Xie X-B, Shi Q-S, Zeng H-Y, Ou-Yang Y-S, Chen Y-B. Antibacterial Activity and Mechanism of Silver Nanoparticles on Escherichia Coli. Appl Microbiol Biotechnol 2010, 85 (4), 1115–1122. doi:10.1007/s00253-009-2159-5
Akter M, Sikder MdT, Rahman MdM, Ullah AKMA, Hossain KFB, Banik S, Hosokawa T, Saito T, Kurasaki M. A systematic review on silver nanoparticles-induced cytotoxicity: physicochemical properties and perspectives. J Adv Res. 2017;9:1–16. doi:10.1016/j.jare.2017.10.008
Qing Y, Cheng L, Ruiyan L, Liu G, Zhang Y, Tang X, Wang J, Liu H, Qin Y. Potential antibacterial mechanism of silver nanoparticles and the optimization of orthopedic implants by advanced modification technologies. Int J Nanomed. 2018;13. doi:10.2147/IJN.S165125
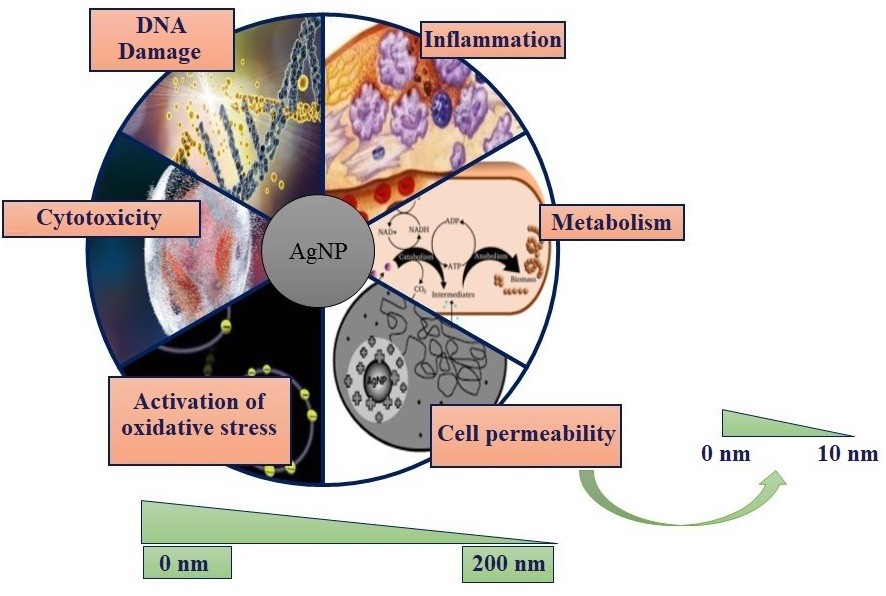
Dakal TC, Kumar A, Majumdar RS, Yadav V. Mechanistic basis of antimicrobial actions of silver nanoparticles. Front Microbiol. 2016;7.
Kowalczyk P, Szymczak M, Maciejewska M, Laskowski Ł, Laskowska M, Ostaszewski R, Skiba G, Franiak-Pietryga I. All that glitters is not silver—a new look at microbiological and medical applications of silver nanoparticles. Int J Mol Sci. 2021;22:854. doi:10.3390/ijms22020854
Fanoro OT, Oluwafemi OS. Bactericidal antibacterial mechanism of plant synthesized silver, gold and bimetallic nanoparticles. Pharm. 2020;12(11):1044. doi:10.3390/pharmaceutics12111044
Lara H, Ayala-Nunez V, Ixtepan Turrent L, Rodríguez-Padilla C. Bactericidal effect of agnps against multidrugresistant bacteria. World J Microbiol Biotechnol. 2009;26:615–621. doi:10.1007/s11274-009-0211-3
Lee MJ, Lee SJ, Yun SJ, Jang J-Y, Kang H, Kim K, Choi I-H, Park S. Silver nanoparticles affect glucose metabolism in hepatoma cells through production of reactive oxygen species. IJN. 2015;11:55–68. doi:10.2147/IJN.S94907
Yin IX, Zhang J, Zhao IS, Mei ML, Li Q, Chu CH. The antibacterial mechanism of silver nanoparticles and its application in dentistry. IJN. 2020;15:2555–2562. doi:10.2147/IJN.S246764
Tang S, Zheng J. Antibacterial activity of silver nanoparticles: structural effects. Adv Health Mater. 2018;7(13):e1701503. doi:10.1002/adhm.201701503
Velusamy P, Su C-H, Venkat Kumar G, Adhikary S, Pandian K, Gopinath SCB, Chen Y, Anbu P. Biopolymers regulate silver nanoparticle under microwave irradiation for effective antibacterial and antibiofilm activities. PLoS One. 2016;11(6):e0157612. doi:10.1371/journal.pone.0157612
Ivask A, ElBadawy A, Kaweeteerawat C, Boren D, Fischer H, Ji Z, Chang CH, Liu R, Tolaymat T, Telesca D, Zink JI, Cohen Y, Holden PA, Godwin HA. Toxicity mechanisms in escherichia coli vary for silver nanoparticles and differ from ionic silver. ACS Nano. 2014;8(1):374–386. doi:10.1021/nn4044047
Gibała A, Żeliszewska P, Gosiewski T, Krawczyk A, Duraczyńska D, Szaleniec J, Szaleniec M, Oćwieja M. Antibacterial and antifungal properties of silver nanoparticles—effect of a surface-stabilizing agent. Biomol. 2021;11(10):1481. doi:10.3390/biom11101481
Haytham MM Ibrahim. Green synthesis and characterization of silver nanoparticles using banana peel extract and their antimicrobial activity against representative microorganisms. J Radiation Res Appl Sci. 2015;8(3):265–275. doi:10.1016/j.jrras.2015.01.007
Lv X, Wang P, Bai R, Cong Y, Suo S, Ren X, Chen C. Inhibitory effect of silver nanomaterials on transmissible virus-induced host cell infections. Biomater. 2014;35(13):4195–4203. doi:10.1016/j.biomaterials.2014.01.054
Jeremiah SS, Miyakawa K, Morita T, Yamaoka Y, Ryo A. Potent antiviral effect of silver nanoparticles on SARS-CoV-2. Biochem Biophys Res Commun. 2020;533(1):195–200. doi:10.1016/j.bbrc.2020.09.018
Sun L, Singh AK, Vig K, Pillai SR, Singh SR. Silver nanoparticles inhibit replication of respiratory syncytial virus. J Biomed Nanotechnol. 2008;4(2):149–158. doi:10.1166/jbn.2008.012
Lu L, Sun R, Chen R, Hui C-K, Ho C-M, Luk J, Lau G, Che C-M. Silver nanoparticles inhibit hepatitis B virus replication. Antiviral Therapy. 2008;13:253–262.
Galdiero S, Falanga A, Vitiello M, Cantisani M, Marra V, Galdiero M. Silver nanoparticles as potential antiviral agents. Molecules. 2011;16(10):8894-8918. doi:10.3390/molecules16108894
Kumar S, Nyodu R, Maurya VK, Saxena SK. Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Coronavirus Disease 2019 (COVID-19). 2020 Apr 30:23–31. doi:10.1007/978-981-15-4814-7_3
Gaikwad S, Ingle A, Gade A, Rai M, Falanga A, Incoronato N, Galdiero S, Galdiero M. Antiviral activity of mycosynthesized silver nanoparticles against herpes simplex virus and human parainfluenza virus type 3. Int J Nanomed. 2013;8:4303–4314. doi:10.2147/IJN.S50070
Chen L, Liang J. An overview of functional nanoparticles as novel emerging antiviral therapeutic agents. Mater Sci Eng C Mater Biol Appl. 2020;112:110924. doi:10.1016/j.msec.2020.110924
Orlowski P, Tomaszewska E, Gniadek M, Baska P, Nowakowska J, Sokolowska J, Nowak Z, Donten M, Celi-chowski G, Grobelny J, Krzyzowska M. Tannic acid modified silver nanoparticles show antiviral activity in herpes simplex virus type 2 infection. PLOS ONE. 2014;9(8):e104113. doi:10.1371/journal.pone.0104113
Mehrbod P, Motamed N, Tabatabaian M, Estyar R, Amini E, Shahidi M, Kheiri M. In vitro antiviral effect of “nanosilver” on influenza virus. DARU J Pharm Sci. 2009;17.
Lin Z, Li Y, Guo M, Xu T, Wang C, Zhao M, Wang H, Chen T, Zhu B. The inhibition of h1n1 influenza virus-induced apoptosis by silver nanoparticles functionalized with zanamivir. RSC Adv. 2017;7(2):742–750. doi:10.1039/C6RA25010F
Nakamura S, Sato M, Sato Y, Ando N, Takayama T, Fujita M, Ishihara M. Synthesis and application of silver nanoparticles (Ag NPs) for the prevention of infection in healthcare workers. Int J Mol Sci. 2019;20(15):3620. doi:10.3390/ijms20153620
Elechiguerra JL, Burt JL, Morones JR, Camacho-Bragado A, Gao X, Lara HH, Yacaman MJ. Interaction of silver nanoparticles with HIV-1. J Nanobiotechnol. 2005;3(1):6. doi:10.1186/1477-3155-3-6
Lara HH, Ixtepan-Turrent L, Garza-Treviño EN, Rodriguez-Padilla C. PVP-coated silver nanoparticles block the transmission of cell-free and cell-associated HIV-1 in human cervical culture. J Nanobiotechnol. 2010;8(1):15. doi:10.1186/1477-3155-8-15
Speshock JL, Murdock RC, Braydich-Stolle LK, Schrand AM, Hussain SM. Interaction of silver nanoparticles with tacaribe Virus. J Nanobiotechnol. 2010;8(1):19. doi:10.1186/1477-3155-8-19
Rogers JV, Parkinson CV, Choi YW, Speshock JL, Hussain SM. A preliminary assessment of silver nanoparticle inhibition of monkeypox virus plaque formation. Nanoscale Res Lett. 2008;3(4):129–133. doi:10.1007/s11671-008-9128-2
El-Sheekh MM, El-Kassas HY. Algal production of nanosilver and gold: their antimicrobial and cytotoxic activities: a review. J Genetic Eng Biotechnol. 2016;14(2):299–310. doi:10.1016/j.jgeb.2016.09.008
Almatroudi A. Silver nanoparticles: synthesis, characterisation and biomedical applications. Open Life Sci. 2020;15(1):819–839. doi:10.1515/biol-2020-0094
Rai M, Kon K, Ingle A, Duran N, Galdiero S, Galdiero M. Broadspectrum bioactivities of silver nanoparticles: the emerging trends and future prospects. Appl Microbiol Biotechnol. 2014;98(5):1951–1961. doi:10.1007/s00253-013-5473-x
Żarowska B, Koźlecki T, Piegza M, Jaros-Koźlecka K, Robak M. New look on antifungal activity of silver nanoparticles (AgNPs). Pol J Microbiol. 2019;68(4):515–525. doi:10.33073/pjm-2019-051
Kim K-J, Sung WS, Moon S-K, Choi J-S, Kim JG, Lee DG. Antifungal effect of silver nanoparticles on dermatophytes. J Microbiol Biotechnol. 2008;18(8):1482–1484.
Suwan T, Khongkhunthian S, Okonogi S. Antifungal activity of polymeric micelles of silver nanoparticles prepared from psidium guajava aqueous extract. Drug Discoveries Therapeutics. 2019;13:62–69. doi:10.5582/ddt.2019.01024
Lotfali E, Toreyhi H, Makhdoomi Sharabiani K, Fattahi A, Soheili A, Ghasemi R, Keymaram M, Rezaee Y, Iranpanah S. Comparison of antifungal properties of gold, silver, and selenium nanoparticles against amphotericin bresistant candida glabrata clinical isolates. Avicenna J Medical Biotechnol. 2020;13(1):47–50. doi:10.18502/ajmb.v13i1.4578
Monteiro D, Silva S, Negri M, Gorup L, Camargo E, Oliveira R, Barros Barbosa D, Henriques M. Silver nanoparticles: influence of stabilizing agent and diameter on antifungal activity against candida albicans and candida glabrata biofilms. Lett Appl Microbiol. 2012;54:383–391. doi:10.1111/j.1472-765X.2012.03219.x
Radhakrishnan VS, Reddy Mudiam MK, Kumar M, Dwivedi SP, Singh SP, Prasad T. Silver nanoparticles induced alterations in multiple cellular targets, which are critical for drug susceptibilities and pathogenicity in fungal pathogen (Candida albicans). Int J Nanomedicine. 2018;13:2647-2663. doi:10.2147/IJN.S150648
Rónavári A, Igaz N, Gopisetty MK, et al. Biosynthesized silver and gold nanoparticles are potent antimycotics against opportunistic pathogenic yeasts and dermatophytes. Int J Nanomedicine. 2018;13:695-703. doi:10.2147/IJN.S152010
Xu Y, Gao C, Li X, He Y, Zhou L, PangbG, Sun S. In Vitro antifungal activity of silver nanoparticles against ocular pathogenic filamentous fungi. J Ocul Pharmacol Ther. 2013;29(2):270–274. doi:10.1089/jop.2012.0155
Mussin JE, Roldán MV, Rojas F, Sosa M de los Á, Pellegri N, Giusiano G. Antifungal activity of silver nanoparticles in combination with ketoconazole against malassezia furfur. AMB Express. 2019;9:131. doi:10.1186/s13568-019-0857-7
Dilshad E, Bibi M, Sheikh NA, Tamrin KF, Mansoor Q, Maqbool Q, Nawaz M. Synthesis of functional silver nanoparticles and microparticles with modifiers and evaluation of their antimicrobial, anticancer, and antioxidant activity. J Funct Biomater. 2020;11(4):76. doi:10.3390/jfb11040076
Farrag HMM, Mostafa FAAM, Mohamed ME, Huseein EAM. Green biosynthesis of silver nanoparticles by aspergillus niger and its antiamoebic effect against allovahlkampfia spelaea trophozoite and cyst. Exp Parasitol. 2020;219:108031. doi:10.1016/j.exppara.2020.108031
Allahverdiyev AM, Abamor ES, Bagirova M, Ustundag CB, Kaya C, Kaya F, Rafailovich M. Antileishmanial effect of silver nanoparticles and their enhanced antiparasitic activity under ultraviolet light. Int J Nanomed. 2011;6:2705–2714. doi:10.2147/IJN.S23883
Fanti JR, Tomiotto-Pellissier F, Miranda-Sapla MM, et al. Biogenic silver nanoparticles inducing Leishmania amazonensis promastigote and amastigote death in vitro. Acta Trop. 2018;178:46-54. doi:10.1016/j.actatropica.2017.10.027
Mayelifar K, Taheri AR, Sazgarnia A. Ultraviolet B efficacy in improving antileishmanial effects of silver nanoparticles. Iran J Basic Medical Sci. 2015;18:677–683. doi:10.1016/j.actatropica.2017.10.027
Vergara-Duque D, Cifuentes-Yepes L, Hincapie-Riaño T, Clavijo-Acosta F, Juez-Castillo G, Valencia-Vidal B. Effect of Silver Nanoparticles on the Morphology of Toxoplasma gondii and Salmonella braenderup. J Nanotechnol. 2020;2020:9483428. doi:10.1155/2020/9483428
Norouzi R, Ataei A, Hejazy M, Noreddin A, El Zowalaty ME. Scolicidal Effects of Nanoparticles Against Hydatid Cyst Protoscolices in vitro. Int J Nanomed. 2020;15:1095-1100. doi:10.2147/IJN.S228538
Azzam A, Saad A, Soliman M, Bayoumy A. Antiparasitic activity of silver and copper oxide nanoparticles against entamoeba histolytica and cryptosporidium parvum cysts. J Egyp Soc Parasitol. 2015;45:593–602. doi:10.12816/0017920
Costa IN, Ribeiro M, Silva Franco P, da Silva RJ, de Araújo TE, Milián ICB, Luz LC, Guirelli PM, Nakazato G, Mineo JR, Mineo TWP, Barbosa BF, Ferro EAV. Biogenic silver nanoparticles can control toxoplasma gondii infection in both human trophoblast cells and villous explants. Front Microbiol. 2020;11:623947. doi:10.3389/fmicb.2020.623947
Machado LF, Sanfelice RA, Bosqui LR, Assolini JP, Scandorieiro S, Navarro IT, Depieri Cataneo AH, Wowk PF, Nakazato G, Bordignon J, Pavanelli WR, Conchon-Costa I, Costa IN. Biogenic silver nanoparticles reduce adherence, infection, and proliferation of toxoplasma gondii rh strain in hela cells without inflammatory mediators induction. Exp Parasitol. 2020;211:107853. doi:10.1016/j.exppara.2020.107853
Gaafar MR, Mady RF, Diab RG, Shalaby TI. Chitosan and silver nanoparticles: promising antitoxoplasma agents. Exp Parasitol. 2014;143:30–38. doi:10.1016/j.exppara.2014.05.005
Adeyemi OS, Murata Y, Sugi T, Kato K. Inorganic nanoparticles kill toxoplasma gondii via changes in redox status and mitochondrial membrane potential. Int J Nanomed. 2017;12:1647–1661. doi:10.2147/IJN.S122178
Younis MS, Abououf EA, Ali AE, Abdelhady SM, Wassef RM. In Vitro effect of silver nanoparticles on blastocystis hominis. Int J Nanomed. 2020;15:8167–8173. doi:10.2147/IJN.S272532
Albalawi AE, Alanazi AD, Baharvand P, Sepahvand M, Mahmoudvand H. High potency of organic and inorganic nanoparticles to treat cystic echinococcosis: an evidence-based review. Nanomater. 2020;10(12):E2538. doi:10.3390/nano10122538
Nassef NE, Saad A-GE, Harba NM, Beshay EVN, Gouda MA, Shendi SS, Mohamed ASED. Evaluation of the therapeutic efficacy of albendazoleloaded silver nanoparticles against echinococcus granulosus infection in experimental mice. J Parasit Dis. 2019;43(4):658–671. doi:10.1007/s12639-019-01145-z
Said DE, Elsamad LM, Gohar YM. Validity of silver, chitosan, and curcumin nanoparticles as antigiardia agents. Parasitol Res. 2012;111(2):545–554. doi:10.1007/s00436-012-2866-1
Mnkandhla D, Marwijk J, Hoppe H, Wilhelmi BS, Whiteley CG. In vivo; in vitro interaction of silver nanoparticles with leucine aminopeptidase from human and plasmodium falciparum. J Nanosci Nanotechnol. 2018;18(2):865–871. doi:10.1166/jnn.2018.13966
Hendiger EB, Padzik M, Sifaoui I, Reyes-Batlle M, López-Arencibia A, Rizo-Liendo A, Bethencourt-Estrella CJ, Nicolás-Hernández DS, Chiboub O, Rodríguez-Expósito RL, Grodzik M, Pietruczuk-Padzik A, Stępień K, Olędzka G, Chomicz L, Piñero JE, Lorenzo-Morales J. Silver nanoparticles as a novel potential preventive agent against acanthamoeba keratitis. Pathogen. 2020;9(5):E350. doi:10.3390/pathogens9050350
Xie Y, Bagby TR, Cohen MS, Forrest ML. Drug delivery to the lymphatic system: importance in future cancer diagnosis and therapies. Expert Opin Drug Deliv. 2009;6(8):785–792. doi:10.1517/17425240903085128
Mathur P, Jha S, Ramteke S, Jain NK. Pharmaceutical aspects of silver nanoparticles. Artif Cells Nanomed Biotechnol. 2018;46:115–126. doi:10.1080/21691401.2017.1414825
De Matteis V, Cascione M, Toma CC, Leporatti S. Silver nanoparticles: synthetic routes, in vitro toxicity and theranostic applications for cancer disease. Nanomater. 2018;8(5):319. doi:10.3390/nano8050319
Dejean L, Martinez-Caballero S, Kinnally K. Is MAC the knife that cuts cytochrome c from mitochondria during apoptosis? Cell Death Differ. 2006;13:1387–1395. doi:10.1038/sj.cdd.4401949
Franco-Molina MA, Mendoza-Gamboa E, Sierra-Rivera CA, Gómez-Flores RA, Zapata-Benavides P, Castillo-Tello P, Alcocer-González JM, Miranda-Hernández DF, Tamez-Guerra R. S, Rodríguez-Padilla C. Antitumor activity of colloidal silver on mcf-7 human breast cancer cells. J Exp Clin Cancer Res. 2010;29(1):148. doi:10.1186/1756-9966-29-148
Ahamed M, Akhtar MJ, Khan MAM, Alhadlaq HA. A Novel Green Preparation of Ag/RGO Nanocomposites with Highly Effective Anticancer Performance. Polym. 2021;13(19):3350. doi:10.3390/polym13193350
Packirisamy G, Gogoi S, Chattopadhyay A, Ghosh S. Implications of silver nanoparticle induced cell apoptosis for in vitro gene therapy. Nanotechnol. 2008;19:075104. doi:10.1088/0957-4484/19/7/075104
Abdel-Fattah W, Ghareib W. On the anticancer activities of silver nanoparticles. J Appl Biotechnol Bioeng. 2018;5. doi:10.15406/jabb.2018.05.00116
AshaRani PV, Low Kah Mun G, Hande MP, Valiyaveettil S. Cytotoxicity and genotoxicity of silver nanoparticles in human cells. ACS Nano. 2009;3(2):279–290. doi:10.1021/nn800596w
Ratan ZA, Haidere MF, Nurunnabi Md, Shahriar SMd, Ahammad AJS, Shim YY, Reaney MJT, Cho JY. Green chemistry synthesis of silver nanoparticles and their potential anticancer effects. Cancers. 2020;12(4):855. doi:10.3390/cancers12040855
Kemp M, Kumar A, Mousa S, Dyskin E, Yalcin M, Ajayan P, Linhardt R, Mousa S. Gold and silver nanoparticles conjugated with heparin derivative possess antiangiogenesis properties. Nanotechnol. 2009:20:455104. doi:10.1088/0957-4484/20/45/455104
Gurunathan S, Lee K-J, Kalishwaralal K, Sheikpranbabu S, Vaidyanathan R, Eom S. antiangiogenic properties of silver nanoparticles. Biomater. 2009;30:6341–6350. doi:10.1016/j.biomaterials.2009.08.008
Yang T, Yao Q, Cao F, Liu Q, Liu B, Wang X-H. Silver nanoparticles inhibit the function of hypoxiainducible factoria1 and target genes: insight into the cytotoxicity and antiangiogenesis. Int J Nanomed. 2016;11:6679–6692. doi:10.2147/IJN.S109695
Sanpui P, Chattopadhyay A, Ghosh S. Induction of apoptosis in cancer cells at low silver nanoparticle concentrations using chitosan nanocarrier. ACS Appl Materi Interfaces. 2011;3:218–228. doi:10.1021/am100840c
Barbalinardo M, Caicci F, Cavallini M, Gentili D. Protein corona mediated uptake and cytotoxicity of silver nanoparticles in mouse embryonic fibroblast small. Nanomater. 2018;14(34):e1801219. doi:10.1002/smll.201801219
Cunningham B, Engstrom AM, Harper BJ, Harper SL, Mackiewicz MR. Silver nanoparticles stable to oxidation and silver ion release show size-dependent toxicity in vivo. Nanomater. 2021;11(6):1516. doi:10.3390/nano11061516
Ferreira LAB, Garcia-Fossa F, Radaic A, Durán N, Fávaro WJ, de Jesus MB. Biogenic silver nanoparticles: in vitro and in vivo antitumor activity in bladder cancer. Eur J Pharm Biopharm. 2020;151:162–170. doi:10.1016/j.ejpb.2020.04.012
Chen Y, Yang T, Chen S, Qi S, Zhang Z, Xu Y. Silver nanoparticles regulate autophagy through lysosome injury and cell hypoxia in prostate cancer cells. J Biochem Molec Toxicol. 2020;34(5):e22474. doi:10.1002/jbt.22474
Xiao H, Chen Y, Alnaggar M. Silver nanoparticles induce cell death of colon cancer cells through impairing cytoskeleton and membrane nanostructure. Micron. 2019;126:102750. doi:10.1016/j.micron.2019.102750
Huy TQ, Huyen PTM, Le A-T, Tonezzer M. Recent advances of silver nanoparticles in cancer diagnosis and treatment. Anticancer Agents Med Chem. 2020;20(11):1276–1287. doi:10.2174/1871520619666190710121727
Xu L, Wang YY, Huang J, Chen CY, Wang ZX, Xie H. Silver nanoparticles: Synthesis, medical applications and biosafety. Theranostics. 2020;10(20):8996-9031. doi:10.7150/thno.45413
Skonieczna M, Hudy D. Biological Activity of Silver Nanoparticles and Their Applications in Anticancer Therapy; IntechOpen, 2018. https://doi.org/10.5772/intechopen.77075.
Bahadar H, Maqbool F, Niaz K, Abdollahi M. Toxicity of nanoparticles and an overview of current experimental models. Iran Biomed J. 2016;20(1):1–11. doi:10.7508/ibj.2016.01.001
Ferdous Z, Nemmar A. Health impact of silver nanoparticles: a review of the biodistribution and toxicity following various routes of exposure. Int J Mol Sci. 2020;21(7):2375. doi:10.3390/ijms21072375
Lee JH, Kim YS, Song KS, Ryu HR, Sung JH, Park JD, Park HM, Song NW, Shin BS, Marshak D, Ahn K, Lee JE, Yu IJ. Biopersistence of silver nanoparticles in tissues from sprague–dawley rats. Particle Fibre Toxicol. 2013;10(1):36. doi:10.1186/1743-8977-10-36
Wen H, Dan M, Yang Y, Lyu J, Shao A, Cheng X, Chen L, Xu L. Acute toxicity and genotoxicity of silver nanoparticle in rats. PLoS One. 2017;12(9):e0185554. doi:10.1371/journal.pone.0185554
Kim K-T, Tanguay RL. The role of chorion on toxicity of silver nanoparticles in the embryonic zebrafish assay. Environ Health Toxicol. 2014;29:e2014021. doi:10.5620/eht.e2014021
Fewtrell L, Majuru B, Hunter PR. A reassessment of the safety of silver in household water treatment: rapid systematic review of mammalian in vivo genotoxicity studies. Environ Health. 2017;16(1):66. doi:10.1186/s12940-017-0279-4
Li Y, Cummins E. Hazard characterization of silver nanoparticles for human exposure routes. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2020;55(6):704-725. doi:10.1080/10934529.2020.1735852
Antony JJ, Sivalingam P, Chen B. Toxicological effects of silver nanoparticles. Environ Toxicol Pharmacol. 2015;40(3):729–732. doi:10.1016/j.etap.2015.09.003
Zou J, Feng H, Mannerström M, Heinonen T, Pyykkö I. Toxicity of silver nanoparticle in rat ear and BALB/c 3T3 cell line. J Nanobiotechnol. 2014;12:52. doi:10.1186/s12951-014-0052-6
Almofti MR. Silver ion induces a cyclosporine a-insensitive permeability transition in rat liver mitochondria and release of apoptogenic cytochrome. J Biochem. 2003;134(1):43–49. doi:10.1093/jb/mvg111
Cho Y-M, Mizuta Y, Akagi J, Toyoda T, Sone M, Ogawa K. Size-dependent acute toxicity of silver nanoparticles in mice. J Toxicol Pathol. 2018;31(1):73–80. doi:10.1293/tox.2017-0043
Sánchez-López E, Gomes D, Esteruelas G, Bonilla L, Lopez-Machado AL, Galindo R, Cano A, Espina M, Ettcheto M, Camins A, Silva AM, Durazzo A, Santini A, Garcia ML, Souto EB. Metal-based nanoparticles as antimicrobial agents: an overview. Nanomater. 2020;10(2):292. doi:10.3390/nano10020292
Liao C, Li Y, Tjong SC. Bactericidal and cytotoxic properties of silver nanoparticles. Int J Mol Sci. 2019;20(2):449. doi:10.3390/ijms20020449
Huang C-L, Hsiao I-L, Lin H-C, Wang C-F, Huang Y-J, Chuang C-Y. Silver nanoparticles affect on gene expression of inflammatory and neurodegenerative responses in mouse brain neural cells. Environ Res. 2015;136:253–263. doi:10.1016/j.envres.2014.11.006
Lin C-X, Yang S-Y, Gu J-L, Meng J, Xu H-Y, Cao J-M. The acute toxic effects of silver nanoparticles on myocardial transmembrane potential, INa and IK1 channels and heart rhythm in mice. Nanotoxicol. 2017;11(6):827–837. doi:10.1080/17435390.2017.1367047
Sung JH, Ji JH, Yoon JU, Kim DS, Song MY, Jeong J, Han BS, Han JH, Chung YH, Kim J, Kim TS, Chang HK, Lee EJ, Lee JH, Yu IJ. Lung Function changes in sprague-dawley rats after prolonged inhalation exposure to silver nanoparticles. Inhal Toxicol. 2008;20(6):567–574. doi:10.1080/08958370701874671
Amreddy N, Babu A, Muralidharan R, Panneerselvam J, Srivastava A, Ahmed R, Mehta M, Munshi A, Ramesh R. Recent advances in nanoparticle-based cancer drug and gene delivery. Adv Cancer Res. 2018;137:115–170. doi:10.1016/bs.acr.2017.11.003
Levard C, Hotze EM, Colman BP, Dale AL, Truong L, Yang XY, Bone AJ, Brown GE, Tanguay RL, Di Giulio RT, Bernhardt ES, Meyer JN, Wiesner MR, Lowry GV. Sulfidation of silver nanoparticles: natural antidote to their toxicity. Environ Sci Technol. 2013;47(23):13440–13448. doi:10.1021/es403527n
Abbasi E, Milani M, Fekri Aval S, Kouhi M, Akbarzadeh A, Tayefi Nasrabadi H, Nikasa P, Joo SW, Hanifehpour Y, Nejati-Koshki K, Samiei M. Silver nanoparticles: synthesis methods, bioapplications and properties. Crit Rev Microbiol. 2016;42(2):173–180. doi:10.3109/1040841X.2014.912200
DOI: https://doi.org/10.15826/chimtech.2022.9.4.02
Copyright (c) 2022 Anton N. Kodintcev

This work is licensed under a Creative Commons Attribution 4.0 International License.
Chimica Techno Acta, 2014–2025
eISSN 2411-1414
Copyright Notice







